Previously, we have discussed both the utility of Vastus Medialis Obliquus strengthening in the treatment of Patellofemoral Pain Syndrome (PFPS) and the underlying biomechanical etiology of PFPS. If the literature has shown focusing on local factors (VMO) to be ineffective, what can you do to help your patients with this painful condition?
Posterolateral Hip Musculature Strengthening
Last year, two systematic reviews revealed further evidence linking weak hip abductors and PFPS.
- PFPS patients showed significantly weaker hip abductors and external rotators when adjusted to the patient’s body weight.1
- In PFPS patients, gluteus medius muscle activity was delayed and of shorter duration during stair ascent/descent and running. In contrast, gluteus maximus muscle activity was increased during stair descent.2
With these findings, it makes sense to target both the hip abductors and external rotators, but is there evidence to support this?
Short-Term Effects of Hip Strengthening
In 2010, a randomized controlled trial compared the short-term effects of a combined hip abductor, lateral rotator, and quadriceps strengthening program to that of a traditional quadriceps strengthening.3 After 4 weeks, those in the first group showed significantly superior improvements in function and reduced pain during stair negotiation.
An earlier study found very similar results.4 As shown in the table below, the control group focused on stretching the quadriceps, gastrocnemius, iliotibial band, and strengthening the quadriceps. The intervention group worked on strengthening for the transverse abdominal muscles and the hip abductors/rotators. Only the intervention group improved perceived pain symptoms during functional activities.
These studies show targeted hip strengthening as a viable option, but unfortunately, only provide outcomes between 4 and 6 weeks post intervention.
Long-Term Effects of Isolated Hip Strengthening
Khayambashi et al conducted a randomized controlled trial looking at isolated hip abductor and external rotator strengthening performed 3 times per week for 8 weeks with a 6-month follow-up.5 At the conclusion of the study, the exercise group’s pain (visual analog scale) and health status (WOMAC) have significantly improved in comparison to both baseline and the control group (as shown in the table 1).
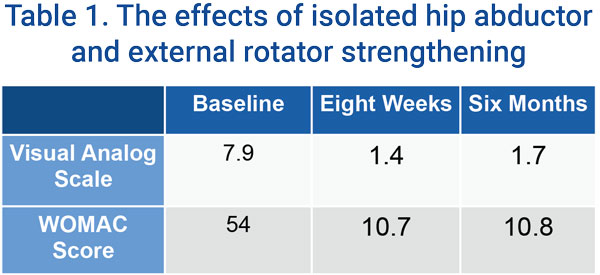
This study showed the utility of hip posterolateral musculature training in isolation from any other intervention.
Combining Hip Strengthening and a Knee Exercise Program
To build upon this study, Fukuda et al attempted to determine if adding hip strengthening exercises to a conventional knee exercise program produced better long-term outcomes than conventional knee exercises alone.6
Once again, the experimental group showed superior results in comparison to the traditional quadriceps strengthening program. The combined hip/knee strengthening program produced significant improvements in all outcome measures (LEPS, AKPS, Single-hop test, and NPRS ascending/descending stairs) at 3, 6, and 12 months post-treatment. In comparison, the traditional quadriceps program only showed decreases in pain at 3 and 6 months.
The body of evidence supporting the targeted strengthening of the hip abductors and external rotators continues to grow with documented short- and long-term functional and pain-specific outcomes.
Pain Reduction in Hip Strengthening Programs
Dolak et al determined that those who completed a hip-specific strength program prior to progressing to a functional strength program demonstrated increased pain reduction compared to those who completed a quadriceps-specific strength program.7 The hip-specific group’s VAS Pain Score decreased from 4.6 to 2.4, while the quadriceps-specific group only decreased from 4.2 to 4.1.
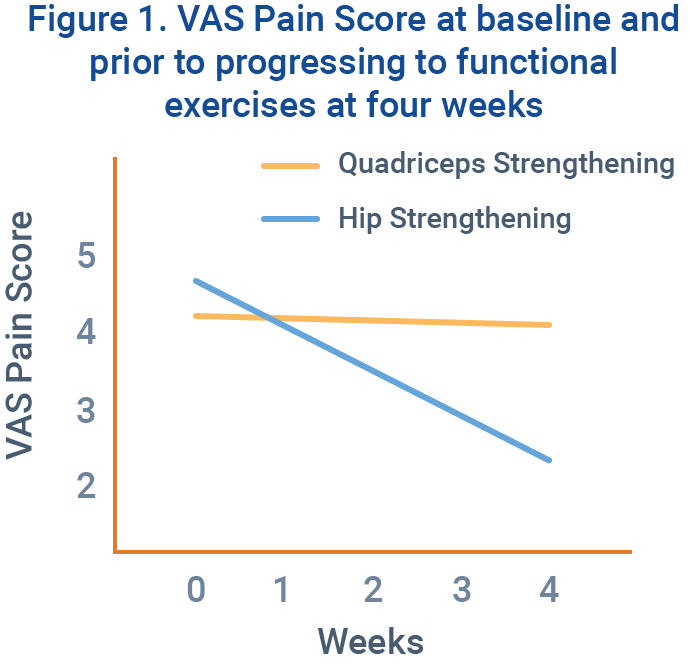
This study shows the importance of controlling frontal and transverse plane movements prior to beginning an intensive functional strength program.
For further information regarding hip abductor (specifically gluteus medius) strength training, please read “Evidence-Based Strength Training: Gluteus Medius.“
Quadriceps Musculature Strengthening
As common sense would dictate, Lankhorst et al found quadriceps weakness to be a risk factor for developing PFPS.8 However, quadriceps strengthening with this patient population is an especially difficult task, because patellofemoral joint stress is of utmost importance during rehabilitation.
PFJ Stress and Knee Flexion
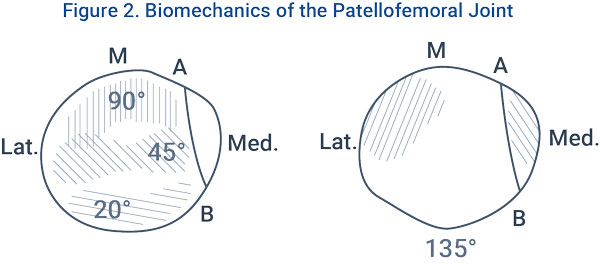
According to Steinkamp et al, patellofemoral joint stress increases with decreasing angles of knee flexion in the open kinetic chain (OKC).9 However, stress also increases with increasing levels of knee flexion in the closed kinetic chain (CKC). Thus, the most appropriate exercise ranges for those with PFPS are 0-45° in the CKC and 90-45° in the OKC.
Joint Contact Area
Chondral lesions and osteoarthritic changes are common within this population, so you must pay close attention to where the joint contact area migrates during exercise. As knee flexion increases, the patella glides inferiorly on the femur, while contact on the patella gradually shifts from inferior to superior.
This information aids us in exercise prescription, but it should not eliminate other ranges of motion during rehab. Pain is patient-specific and can vary based on underlying pathology, experiences, and other biomechanical/neurophysiological factors. All exercises should be conducted within your individual patient’s tolerance and these ‘appropriate ranges’ should be used to help guide your prescription.
Functional Exercises and PFJ Stress
Upon implementing a more functional approach (which should be started as soon as possible), patellofemoral joint stress and patient response to treatment should continue to guide your program.
Chinkulprasert et al conducted a controlled laboratory study to determine what exercises elicit the greatest patellofemoral joint stresses among the lateral step-up, forward step-up, and forward step-down.10 The three exercises were performed by 20 healthy subjects at the same step height. The study concluded that significantly greater patellofemoral stresses and reaction forces were recorded during the forward step-down than during the other two exercises.
Early in rehabilitation, the forward step-down should be withheld in favor of the less intense exercises. As patient tolerance increases, the forward step-down can be a viable option to improve eccentric quadriceps control during stair ascent.
By understanding the current literature and basic biomechanics involved in PFPS, clinician are better able to safely and effectively manage their patients’ symptoms and return them to the sport or recreational activities that they enjoy.


No Comments to "PFPS Treatment: Hip and Quadriceps Strengthening"